Medical Clinic
We use state-of-the-art medical equipment to ensure effective and safe treatments.
Prostate Adenoma Treatment
What Does the Treatment for Prostate Adenoma Involve?

When medication therapy no longer provides the expected results, meaning the patient begins to experience recurrent urinary tract infections, or bladder stones develop, or ultrasound shows that the bladder is no longer emptying completely, or even acute retention or urinary blockage occurs, surgical treatment options become necessary.
When a man experiences one of the symptoms of prostate adenoma, there are several options regarding the treatment of this condition:
Medication Treatment
It represents a first option in the treatment of prostate adenoma. This method is effective in patients with mild to moderate symptoms and is limited over time, as the medication can provide beneficial effects for a period of up to 10–15 years.
Alpha-blockers are the first type of medication prescribed by the urologist. They relax the muscles inside the prostate and the bladder neck, facilitating the passage of urine. They may cause side effects such as low blood pressure, difficult or absent ejaculation, and nasal congestion.
5-alpha reductase inhibitors: They reduce the volume of the prostate gland (recommended for prostates larger than 50 cm³) and can be used together with alpha-blockers if the PSA level is higher than 1.5 ng/ml (a possible indicator that the prostate is significantly enlarged). These medications may cause erectile or libido problems. The effect of 5-alpha reductase inhibitors is noticeable after 6 months of treatment. They also reduce PSA levels by more than 50%.
In cases of prostate enlargement, the combination of both types of medication is more effective in reducing the risk of complications (particularly urinary retention) and lowering the likelihood of surgical intervention.
When medication therapy no longer provides the expected results, meaning the patient begins to experience recurrent urinary tract infections, or bladder stones develop, or ultrasound shows that the bladder is no longer emptying completely, or even acute retention or urinary blockage occurs, surgical treatment options become necessary.

2. Surgical Treatment
There are several options regarding this type of treatment:
2.1 Classical surgical intervention
It is very rarely used today, being reserved only for certain cases of very large prostate adenomas (150–200 cm³). It involves an abdominal incision and opening of the pelvic cavity, with the complete instrumental removal of the prostate.
It requires a long hospital stay (usually at least 14 days), a prolonged healing time for the abdominal wound, and carries a higher risk of postoperative bleeding.
2.2 Endoscopic interventions
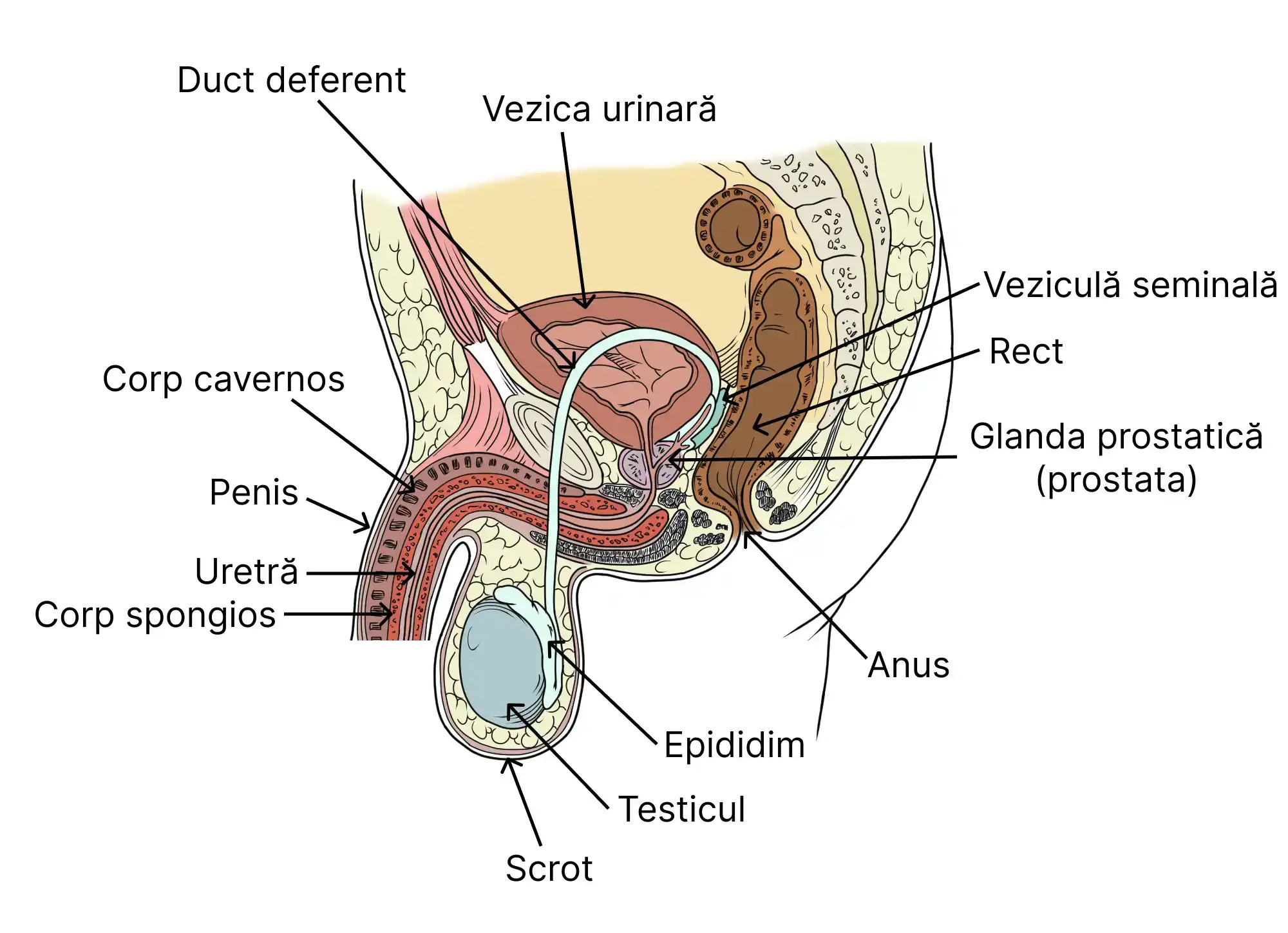
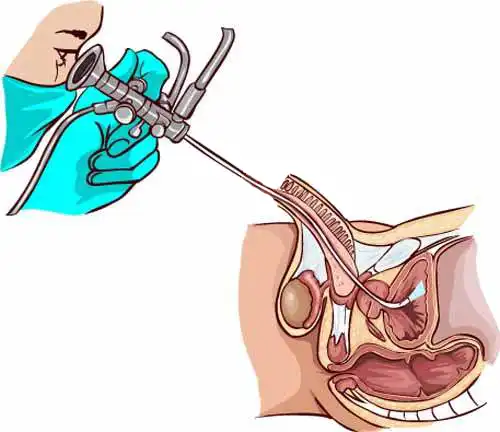
This type of surgical intervention has been in routine use for about 20–25 years and involves the removal of prostate adenoma through a minimally invasive surgical technique, in which an instrument (endoscope, resectoscope) is inserted through a natural pathway of the body (the urethra) to the area compressed by the excess prostatic tissue. The urologist then removes this tissue using various resection methods (high-frequency electric current, laser, or pressurized water vapor).
These treatments are much easier for the patient to tolerate and require significantly shorter hospital stays (5–7 days in the case of resection with electric current or laser, or even just a few hours in the case of water vapor resection).
As can be seen in the image, the anatomy of the pelvis and urethra ideally allows minimally invasive endoscopic access (without skin incision) through the natural urinary evacuation channel (the urethra) to the prostate, for the purpose of its removal.
As shown in the image below, by using the endoscopic technique, the urologist has continuous direct optical access to the surgical field (or via a video camera attached to the endoscopic instrument, which transmits the image of the surgical field to a monitor in the operating room).
The main types of endoscopic intervention for prostate adenoma
I. Transurethral resection of the prostate (TURP) – with laser or bipolar electric current, indicated for a prostate volume between 40 and 80–100 cm³.
This medical procedure involves an endoscopic intervention, which requires the insertion of a metal instrument equipped with a video camera. The instrument has a sliding component, represented by a metal loop through which a high-frequency electric current passes, cutting and excising sections of the prostate. The procedure lasts 1–2 hours, is performed under anesthesia (spinal or deep sedation), and requires a hospital stay of 4–10 days, during which the patient undergoes treatment and has a catheter inserted through the urethra to aid the healing process.
It is a surgical method that has been widely used for about 20–25 years.
ADVANTAGES: Rapid improvement in urinary flow, occurring immediately in the postoperative period. Recovery period of approximately 1 month after the procedure.
In the video animation below, you can see how a TURP procedure is performed, as well as how the surgical loop carrying an electric current gradually cuts sections of the prostate, which are then released into the bladder and later removed through irrigation with saline solution via a wide-diameter catheter. The main drawback of this type of intervention can also be observed—namely, the repeated bleeding that inevitably occurs when the electric loop cuts through portions of the prostate. These bleedings are immediately coagulated with the same electric loop, but the risk of bleeding restarting at any time in the immediate postoperative period is quite high, which is why a postoperative hospital stay under strict supervision for 5–7 days is necessary.
II. Prostate Vaporization Procedure with Steam Vapors
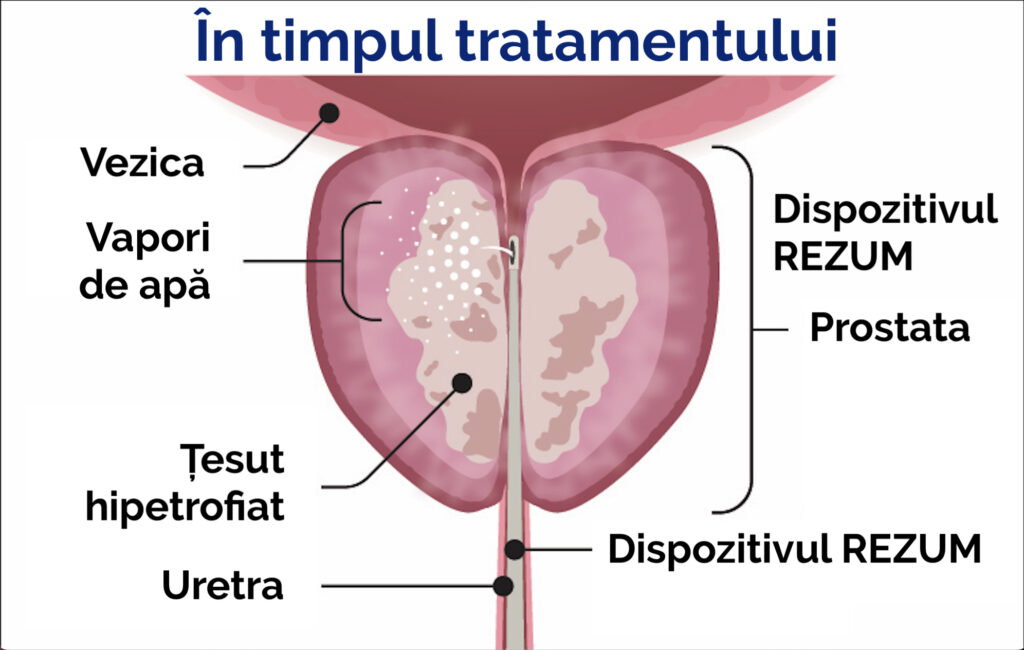
This is a relatively recent medical procedure (first performed in Romania by the doctors of Ro-Boost Clinic—Dr. Bogdan Gusanu in 2021 and Dr. Emanuel Alexandrescu in 2022, at Med-As Victoria Hospital). It also involves an endoscopic intervention, using an instrument similar to that employed in TURP, but equipped at its tip with a very fine needle. With this needle, a series of punctures (4–10) are made into the prostate, through which pressurized water vapor is injected. Once injected, the water vapor causes the prostatic tissue to atrophy and gradually disappear, a process that unfolds over a period of 2–3 months after the intervention. The procedure is minimally invasive, usually requires only local anesthesia or sedation (putting the patient to sleep for 15–20 minutes), and can be performed either on an outpatient basis or in hospital, requiring hospitalization for up to 12 hours.

ADVANTAGES:
– no intraoperative or postoperative bleeding;
– no retrograde ejaculation;
– no erectile dysfunction;
– the procedure can be performed on an outpatient basis or with hospitalization of up to 12 hours;
– local anesthesia or sedation.
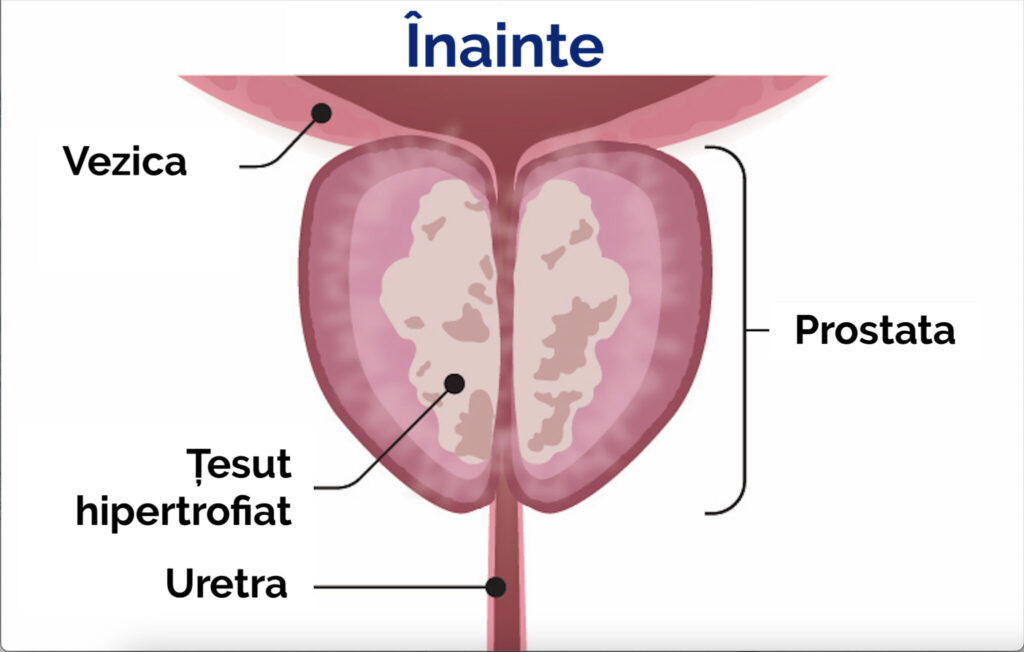
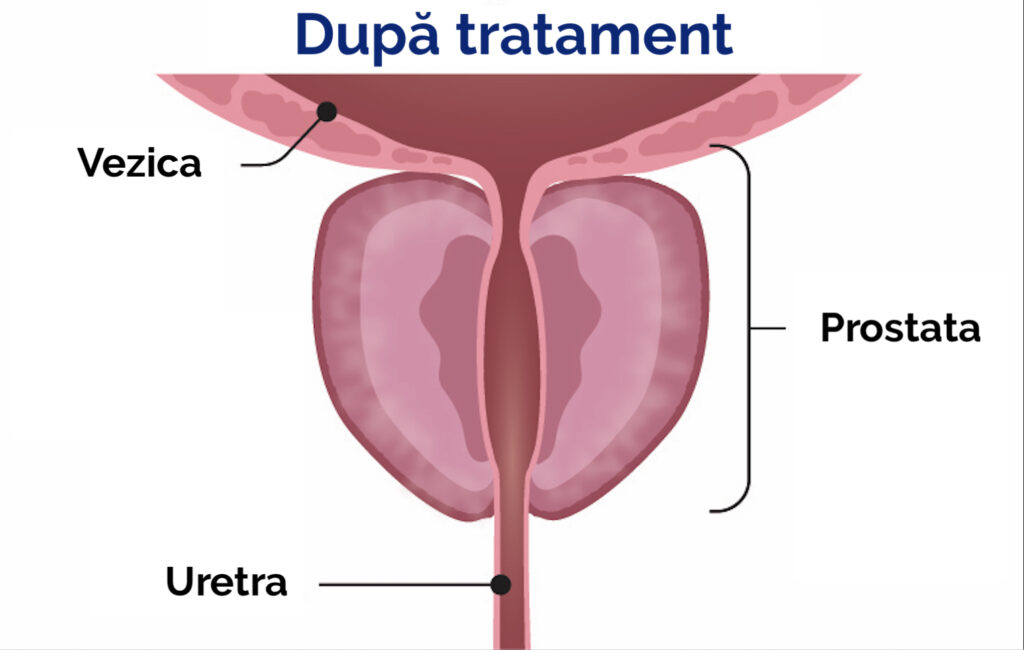
In the images below, one can observe the considerable widening of the urethral caliber (and thus the improvement of urinary flow) after the procedure, as the prostatic tissue undergoes atrophy.
Technical Considerations on the Prostate Vaporization Procedure Using Steam Vapors
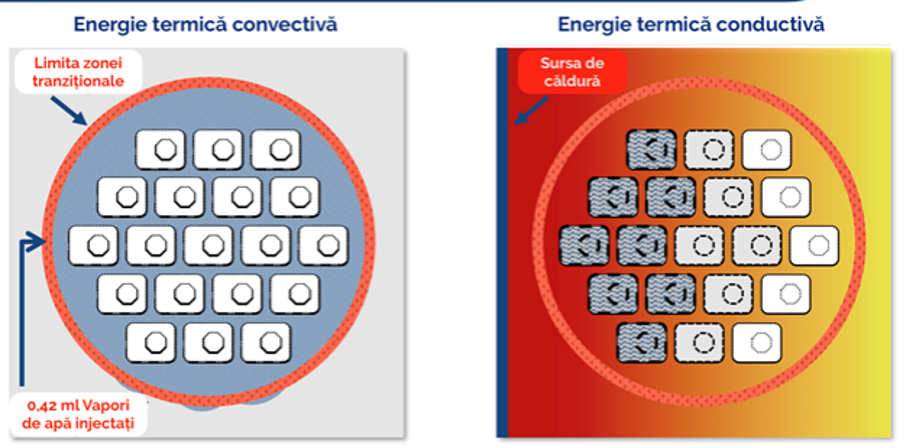
A precise dose of thermal energy from water vapor is delivered into the prostate tissue using a small needle with multiple emitter holes, allowing controlled and uniform vapor dispersion.
The vapor is administered into the targeted tissue at slightly above interstitial pressure, convectively driving the water vapor through the tissue interstices, where it condenses and transfers the stored thermal energy directly to the targeted tissue.
This convective heat transfer is what distinguishes this technique from other ablative thermal therapies, which rely on the slower, less precise, and less efficient process of conductive heat transfer to the tissue.
The convective transfer of thermal energy from the water vapor to the tissue is rapid but also self-limiting. As the water vapor disperses through the tissue, it condenses back into its liquid state, ensuring that the energy does not extend beyond the intended treatment area.
The prostate vaporization system is powered by the convective energy of water vapor and delivers targeted, controlled doses of thermal energy—stored within the water vapor—directly into the prostate gland region, specifically into the prostate tissue responsible for lower urinary tract symptoms secondary to benign prostatic hyperplasia.
Each 9-second injection treatment uses 0.42 ml of heated sterile water vapor, which rapidly and evenly disperses through the tissue interstices.
The condensation of water vapor releases the stored thermal energy. Cell membranes are denatured, causing immediate cell death, vascularization is sealed, and alpha-adrenergic nerves in the treatment area are denervated, providing an effective, uniform, and predictable treatment.
Over time, this destroyed tissue is reabsorbed through the body’s natural healing response, reducing the volume of tissue, allowing the urethra to open, and relieving lower urinary tract symptoms.
Advantages of the Prostate Vaporization Procedure Using Steam Vapors
In the video below, you can watch the practical execution of a procedure using the prostate vaporization technique. Note the complete absence of any intraoperative bleeding, which gives this method one of its main advantages over the current TUR-P technology.
Frequently Asked Questions
What Does the Prostate Vaporization Procedure Using Steam Vapors Involve?
We perform the procedure under local anesthesia or sedation.
We insert an endoscope through the urethra into the prostate. This technique is used to guide a visible needle into the prostatic tissue.
Radiofrequency energy is used to heat water and create steam. The steam is dispersed into the prostate tissue through the needle. We usually repeat this process between two and eight times, depending on the size of your prostate.
The heat from the water vapor travels through the enlarged prostate tissue, causing cell death. In the weeks to months following the procedure, the body reabsorbs the dead cells, leading to a shrinkage of the prostate. This relieves the bladder obstruction that causes urinary symptoms.
What Is the Recovery Process After Prostate Vaporization with Steam Vapors?
You will have a catheter after the procedure. The catheter will drain urine into a bag. The urine bag can be attached to your leg and hidden under your pants. The catheter will be removed in our office seven days after the procedure.
After undergoing the prostate vaporization procedure, the body triggers an inflammatory response that initially worsens urinary symptoms. For approximately four weeks following the procedure, it is common to experience burning or stinging sensations during urination. A slow urine flow, as well as increased urgency and frequency, are also typical and may be more pronounced than before the procedure.
You may need to take medication to manage your urinary symptoms for about six weeks after the procedure.
You should notice that urinary symptoms gradually improve between four and twelve weeks after the procedure.
Depending on your job, you may be able to return to work about three days after the procedure, although some men prefer to wait until the catheter has been removed.
You will not be able to drive for at least 24 hours after the procedure. Some men prefer not to drive until the catheter has been removed.
What Are the Benefits of the Prostate Vaporization Procedure with Steam Vapors?
The prostate vaporization procedure is an alternative to long-term medication for urinary symptoms caused by benign enlargement of the prostate.
If you are already taking medication for urinary symptoms, in 90% of cases you will be able to stop the medication after the procedure.
The prostate vaporization procedure can be performed as a day surgery—you may go home on the same day of the procedure, provided you are accompanied by a responsible adult.
Some medications and prostate surgeries can cause retrograde ejaculation. Retrograde ejaculation results in a reduced amount of semen during orgasm (a “dry orgasm”). The risk of retrograde ejaculation after the prostate vaporization procedure is approximately 4–6%, which is lower than with many other treatment options.
Some medications and prostate surgeries can cause erectile dysfunction. The risk of erectile dysfunction after the prostate vaporization procedure is very low.
What Are the Risks of the Prostate Vaporization Procedure with Steam Vapors?
The prostate vaporization procedure is a new surgical technology that had been available only abroad since 2015 and, more recently, in Romania since 2021.
At present, there are no studies that have analyzed the long-term outcomes of the prostate vaporization procedure. It is possible that the benefits of the treatment may diminish over time. For some men, additional treatment for an enlarged prostate may be required in the future.
The improvement of urinary symptoms immediately after the prostate vaporization procedure may not be as rapid as the relief observed with other prostate surgeries, such as transurethral resection of the prostate (TURP) or laser prostatectomy.
As with any surgical procedure, there are potential risks and complications associated with the prostate vaporization procedure:
Bleeding: The risk of blood loss is minimal. The risk of bleeding requiring a blood transfusion is ≤1%.
Infection: ≤5%. Broad-spectrum antibiotics are administered at the beginning of the procedure to minimize the risk of a urinary infection.
Retrograde ejaculation: ≤2%
Erectile dysfunction: ≤2%.
What Are the Possible Immediate Side Effects After the Prostate Vaporization Procedure with Steam Vapors?
Temporary burning and stinging when urinating (which may last 5–7 days) | 1 in 3 patients (33%) |
Temporary blood in the urine (which may last 5–7 days) | 1 in 4 patients (25%) |
Temporary pain or discomfort in the pelvic area | Between 1 in 5 and 1 in 6 patients (16–20%) |
Urinary tract infection requiring antibiotic treatment | 1 in 15 patients (6–7%) |
The procedure may not relieve all of your symptoms, and you may need additional treatment within 4 years. | 1 in 25 patients (approximately 4%) |
The prostate vaporization procedure may be an option for you if:
You do not want to take, or cannot take, medication for an enlarged prostate.
You do not want to undergo a more invasive procedure, such as transurethral resection of the prostate (TURP) or laser prostatectomy.
You do not want a prolonged hospitalization of 5–7 days, with inherent risks of bleeding/infection and subsequent impact on sexual life.
Your prostate is between 30 and 120 grams. (A normally sized prostate is less than 25 grams.)
You prefer to preserve erectile and ejaculatory function, maintaining a normal sexual life after treatment.
www.ro-boost.ro
™ Toate drepturile rezervate.
Address: Bucuresti, strada Dr. Leonte Anastasievici nr. 34, sector 5
Phone: 0743.153.954 | 0743.153.960
Email: contact@ro-boost.ro